TRICARE provides coverage to around 9.6 million beneficiaries in the US. It also offers comprehensive, cost-effective care with TRICARE for Life. They also provide free Medicare wraparound coverage for retirees with Medicare Parts A and B. But do you know how to verify insurance at Tricare-approved residential treatment centers? If not, read ahead and find out!
To verify insurance at Tricare-approved residential treatment centers, contact your TRICARE representative and the treatment center. Contact ChoicePoint at 844.445.2563 for more information.
Table of Contents
Conditions Treated at Tricare-Approved Residential Treatment Centers
Tricare-Approved Residential Treatment Centers aim to serve individuals with substance abuse signs. Addiction treatment is a brave first step towards recovery, and having Tricare insurance can significantly reduce the cost strain. The two main conditions covered by Tricare-approved residential treatment centers are:
Substance Use Disorder
- Detoxification and rehabilitation services are covered through TRICARE-approved residential treatment programs for substance use disorders.
- A primary diagnosis of a drug use disorder with severe or constantly monitored symptoms is required for eligibility.
- To qualify, a person must have a significant disability in several facets of their life.
- Admission to such establishments requires prior authorization.
Mental Illness
- TRICARE-approved psychiatric residential treatment centers offer highly structured, 24-hour therapeutic environments for mental illness.
- Eligibility for this benefit is limited to enrollees under 21 with a significant impairment that hinders daily functioning but doesn’t necessitate hospitalization.
- Transitioning from another program or higher care level may qualify for residential treatment coverage.
- Prior authorization is mandatory for admission to any TRICARE-approved psychiatric residential treatment center.
Co-occurring Disorders
- Tricare-Approved Residential Treatment Centers thoroughly evaluate substance use disorder and underlying mental health conditions.
- The process of rehab combines treatment for mental and physical health
- Different coping mechanisms are provided for long-term recovery at Tricare-Approved Residential Treatment Centers
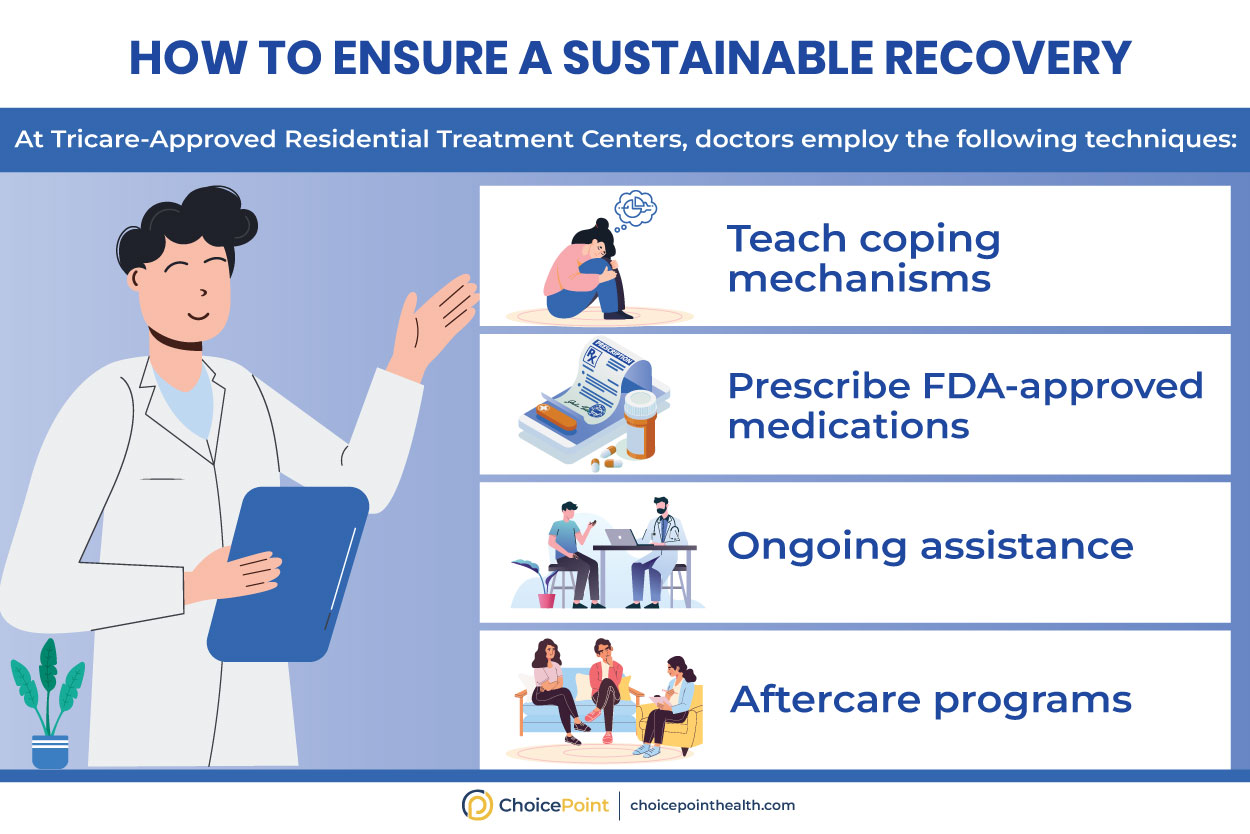
A Sustainable Approach to Addiction Recovery
What Does TRICARE Not Cover?
Although TRICARE offers a wide range of healthcare options, it does have some restrictions and exclusions. Certain coverage details can vary depending on the TRICARE plan a patient may have. Following are some services that TRICARE may not cover:
- Cosmetic Procedures
- Experimental or Investigational Treatments
- Routine dental care for adults
- Elective Eye Surgery(like Lasik etc.)
- Complementary therapies (like acupuncture or chiropractic care )
- Yearly physical exams for adults
Stay updated about Tricare plans, and consult with your TRICARE representative before you begin addiction treatment. At ChoicePoint, our DEA-certified staff helps patients verify insurance. Call 844.445.2563, and stay informed about any updates or changes to your plan’s coverage.
How to Verify Insurance at Tricare-Approved Residential Treatment Centers
Do you want to limit any financial surprises at Tricare-approved residential treatment centers? Here is a step-by-step process of how an individual may verify insurance at Tricare-approved residential treatment centers:
Step#1: Contact TRICARE Representative
The initial step includes contacting a TRICARE representative before signing up for a residential treatment program. Tricare representatives may offer helpful details regarding the specifics of your plan, including
- Network providers
- Any prerequisites
- Authorizations required for addiction treatment
Step#2: Verify TRICARE Approval
Not all residential treatment centers are recognized by TRICARE. It’s crucial to confirm that the institution you’re considering is a Tricare-approved residential treatment center and in-network. You may get the list of Tricare-approved residential treatment centers from your TRICARE representative, or they can assist you in locating one that suits your needs.
Step#3: Determine Eligibility
The next step is to verify that you or a loved one meets the TRICARE addiction treatment coverage requirements. TRICARE eligibility varies depending on elements like:
- Your service status
- Where you live
- The particular plan
Step#4: Preauthorization and Referrals
Before enrolling in Tricare-approved residential treatment centers, some TRICARE plans may require preauthorization or referrals from your primary care physician (PCP). To find out if these actions are required in your situation, you may speak with:
- Your PCP
- TRICARE representative
Step#5: Understand the Costs
Although TRICARE pays for a sizable percentage of the cost of addiction treatment, it’s crucial to be aware of your financial obligations. Examine the specifics of your plan’s coverage, such as:
- Deductibles
- Copayments
- Any out-of-pocket costs you might face while attending a residential treatment facility
Step#6: Contacting the Residential Treatment Center
After ensuring your TRICARE eligibility and coverage, contact a Tricare-approved residential treatment center immediately. The admissions staff at the hospital can help you with:
- Your insurance verification
- Treatment alternatives
- Any queries or issues you may have
Step#7: Gather Necessary Documentation
The admissions procedure can be sped up by having the necessary documents. Before joining the Tricare-approved residential treatment centers, make sure you have the paperwork, including:
- TRICARE ID card
- Evidence of eligibility
- Any necessary preauthorization or referral forms
Step#8: Discuss Payment Arrangements
Even if you have TRICARE coverage, reviewing payment plans with Tricare-approved residential treatment centers is crucial. This entails:
- Verifying their approach to handling insurance claims
- Any up-front fees
- Any potential financial obligations not covered by TRICARE.
Step#9: Keep Records
It is important to keep records in case you ever need to challenge any claims or deal with billing concerns. Keep thorough records of
- All correspondence
- Invoices
- Receipts about your therapy
- Insurance coverage receipts throughout your stay in a residential addiction treatment facility
Did you know that individual plan details, location, legal requirements, and the specific type of treatment sought influence TRICARE coverage for treatment and rehab services?
How Do I Know If I Have Tricare Coverage?
Do you have Tricare coverage? Here is how you may determine if you have TRICARE coverage:
- Confirm your eligibility for TRICARE status on the TRICARE website or by contacting a TRICARE representative.
- Review your enrollment status and plan choice to understand your coverage.
- Your TRICARE ID card contains essential information, like your plan type, group number, and beneficiary number.
- Reach out to TRICARE customer service.
- Log into the TRICARE Online portal to check your coverage details and view claims information.

If you can quit for a day, you can quit for a lifetime,” Benjamin Alire Sáenz said.

If you can quit for a day, you can quit for a lifetime,” Benjamin Alire Sáenz said.
How to Verify Insurance at Tricare-Approved Residential Treatment Centers- Final Words
Verifying insurance at Tricare-Approved Residential Treatment Centers is crucial in receiving the care you or a loved one needs. Following the abovementioned steps, you may confidently handle the process and concentrate on your rehabilitation.
Do you wish to Verify Insurance at Tricare-Approved Residential Treatment Centers without the added burden of finances? Call ChoicePoint now at 844.445.2563!
Q&A Section
Learn about the Tricare-approved residential treatment centers and how to verify insurance;
What Conditions Are Treated at Tricare-Approved Residential Treatment Centers?
Tricare-approved residential treatment centers typically address a range of mental health and substance use disorders.
What Does Tricare Not Cover?
Services and supplies that are not medically or psychologically necessary for the diagnosis or treatment of a covered illness (including mental disorder) or injury or the diagnosis and treatment of pregnancy or well-child care are not covered by TRICARE.
How Do I Know If I Have Tricare Insurance?
Here are some ways:
- Check your Military ID Card for TRICARE eligibility.
- Verify military affiliation with one of the seven uniformed services.
- Visit the official TRICARE website for information.
- Contact TRICARE customer service.
- Review official documentation for TRICARE details.
- Consult with your military command or human resources.
- Check with your sponsor (service member) for eligibility confirmation.
How Do I Check My Tricare Authorization Status?
On the TRICARE West secure patient portal, you can view authorization, status, determination, and letters and make network-to-network provider changes. Web-based portals can also be used to check the status of referrals, authorizations, and claims.
Does Tricare Require a Referral?
Yes, TRICARE often requires a referral for specialty care, depending on the plan and specific circumstances.
Does Tricare cover Suboxone?
Yes, Suboxone is generally covered by TRICARE. However, coverage details may vary depending on the specific TRICARE plan and individual circumstances.
Medical Disclaimer:
ChoicePoint aims to improve the quality of life for people struggling with substance use disorder and mental health issues. Our team of licensed medical professionals research, edit and review the content before publishing. However, this information is not intended to be a substitute for professional medical advice, diagnosis, or treatment. For medical advice please consult your physicians or ChoicePoint's qualified staff.

Start Your Journey Toward Recovery!









Review How to Verify Insurance at Tricare-Approved Residential Treatment Centers.