Are you or a loved one seeking an addiction treatment center offering Medicare inpatient rehab? You’ve come to the right place! This guide will explore all the essential aspects of Medicare’s inpatient rehab coverage. Understanding what is covered and how to utilize these benefits can be vital in accessing the best possible care for your recovery. Whether you’re considering inpatient treatment for yourself or a family member, we’ve covered you with comprehensive information to help you make informed decisions.
Finding a rehab facility that covers all insurance plans has become more accessible. ChoicePoint is here to welcome all who have Medicare inpatient rehab coverage. Reach out to us now and call 844.445.2563.
Table of Contents
What Is Medicare And How To Qualify For Inpatient?
Medicare is a government health insurance program for the people of the United States who are:
- Age 65 or older
- Aged less than 65 with disabilities
- Individuals with End Stage Renal Disease.
To get your Medicare inpatient rehab covered, your doctor needs to verify these points about your condition.
- Need intensive rehab.
- Require ongoing medical supervision.
- Benefit from doctors and therapists working together.
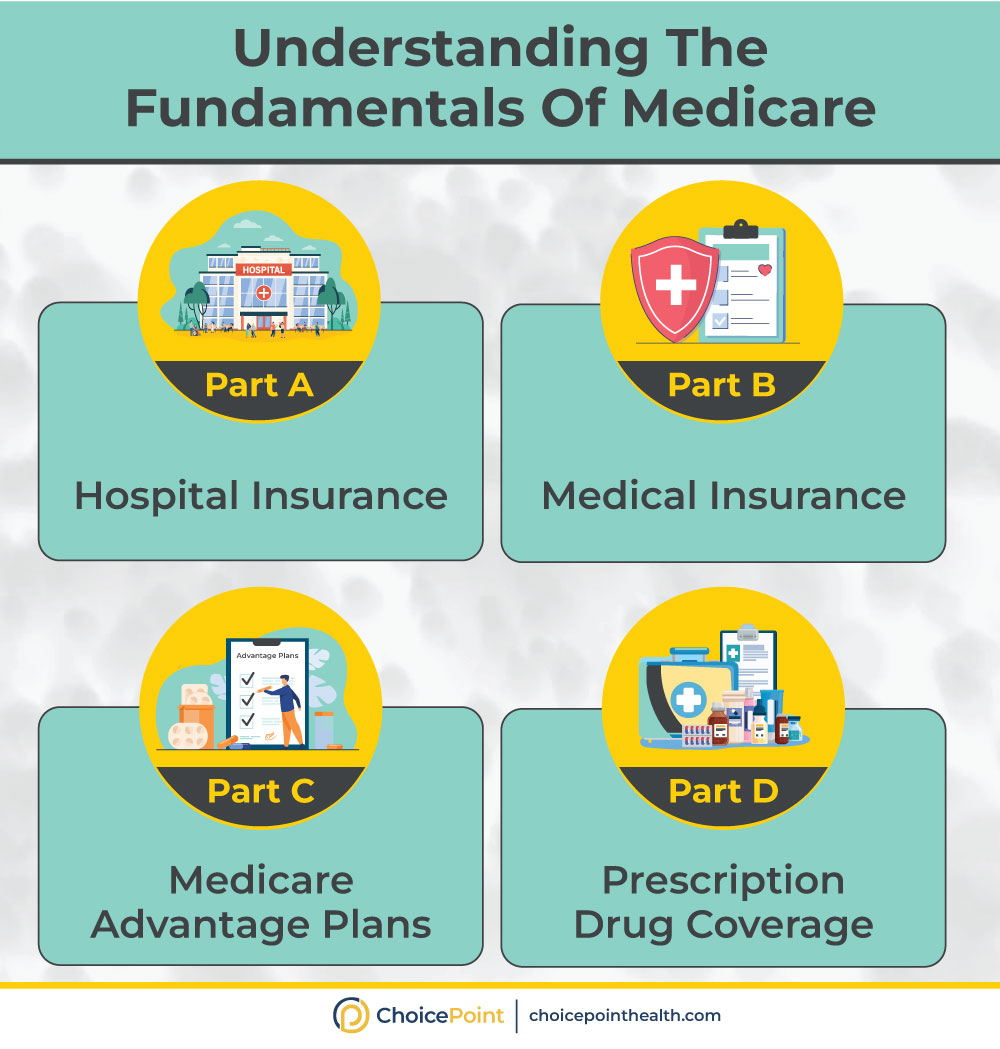
Medicare primarily consists of 3 parts (A, B, and D). Medicare provides comprehensive coverage for various health services, which include:
- Inpatient drug rehab
- Intensive outpatient program
- Outpatient drug rehab
- Partial Hospitalization.
Looking to overcome addiction and break free from destructive habits? Medicare inpatient rehab coverage is a way out. We are here to support you every step of the way. Call us now 844.445.2563.

Paying for Rehab with Medicaid and Medicare
Medicare Inpatient Rehab Coverage for SUDs!
According to a recent study, around 15.35% of Americans have been diagnosed with Substance Use Disorder. Among them, 93.5% did not receive any kind of treatment. Medicare’s got you covered for treating alcoholism and substance use issues. Whether you need help while staying in a facility or getting treatment outside. When you’re in a place for inpatient treatment, Medicare Part A takes care of the expenses, just like any other hospital stay. You’ll deal with the regular co-pays that come with inpatient care.
Medicare covers the following treatment options :
- Detoxification.
- Psychotherapies (CBT, DBT)
- Medication Assisted Treatment
- Opioid Treatment Program
- Toxicology Testing
- Counseling Sessions
- Group Therapies.
- Family Therapies
With all marketplace plans, you can rest assured that insurance providers will cover mental health and substance abuse services as essential health benefits. Regarding Substance Abuse, Medicare may provide some coverage. Medicare inpatient rehab coverage comes under Part A.
It provides coverage for inpatients for up to 190 days. For the initial 60 days, you’ll be responsible for paying the deductible. If your stay exceeds, you must contribute a portion of the expenses. It is best to contact your insurance provider to gain insight into the coverage of Medicare.
Seek help from ChoicePoint, Medicare inpatient rehab, to alleviate the substance use disorder (SUD) burden on you and your family. Call us now 844.445.2563.
What Is Medicare and How Does It Work?
Does Medicare Cover the Opioid Addiction Treatment Plan?
Yes! Medicare inpatient rehab plan may cover treatment for opioid addiction. Opioid Use Disorder is a severe medical condition that needs proper diagnosis and treatment. Medicare Part B covers opioid addiction treatment through Opioid Treatment Programs, known as Suboxone Clinics. Suboxone, an FDA-approved medication, is provided as a part of Medication Assisted Treatment (MAT) to address opioid addiction.
Under Medicare Part B, individuals can access Suboxone treatment. This combines medication with counseling and behavioral therapies, creating a comprehensive approach to recovery. If you or someone you know is struggling with opioid addiction, Suboxone treatment through Medicare can offer a practical and supportive path to overcoming addiction and achieving lasting sobriety.
According to a recent study, the 35-44 years age group is experiencing the most opioid overdose deaths. Services provided at the Opioid treatment program under Medicare coverage are:
- Group therapies
- Indoor activities
- Substance abuse counseling
- Toxicology screening
- Aftercare and Followups
Take back control of your life and break free from the grips of addiction. We are here to support you every step of the way. Take the first step towards understanding your options and securing the healthcare coverage you need.
Medicare Inpatient Rehab Guidelines
The Medicare Inpatient Rehab Guidelines dictate that to qualify for reimbursement, you must have the doctor’s certification for your inpatient stay. To avail of Medicare inpatient rehab services, you must fulfill the following criteria:
- Requirement for Intensive Rehabilitation: The guidelines necessitate a genuine need for intensive rehabilitation to address Substance Use Disorders (SUDs) effectively.
- 24/7 Medical Supervision: Inpatient rehabilitation services under Medicare require facilities to provide round-the-clock medical supervision to ensure patient’s safety and well-being.
- Collaborative Care by DEA-Certified Professionals: Medicare mandates coordinated care involving DEA-certified doctors, therapists, nursing staff, and other qualified healthcare professionals to deliver comprehensive support throughout the rehabilitation process.
Adhering to these guidelines, individuals seek Medicare coverage for inpatient rehab services. And can ensure compliance and receive the necessary support for their recovery journey.
Does Medicare Pay For Inpatients?
Medicare Part A does pay for your inpatient rehabilitation stay like any other regular hospital stay. But, you can expect to put similar out-of-pocket expenses. During your stay at an Inpatient Rehabilitation facility (IRF), Medicare does not cover all aspects of addiction treatment. The positive news is that Medicare covers the entire cost for the initial 60 days of your stay. As a reminder, Medicare inpatient rehab covers expenses up to a maximum of 190 days, a lifetime limit.
Does Medicare Cover Alcohol Rehab?
Yes! Medicare does cover alcohol rehab. However, according to the Affordable Care Act, all insurance providers must cover at least some, if not all, the cost of addiction. So, Medicare will surely provide coverage for alcohol rehab services. If you have Medicare coverage and are dealing with addiction, consider an outpatient rehab. It offers a host of advantages that may surpass those of inpatient treatment.
Does Medicare Cover Outpatient Rehab?
Yes, Medicare does cover outpatient rehab under Medicare Part B. This includes services for substance use disorders and alcoholism. Check your plan for co-payments or deductibles.
Take the first step now toward your journey to sobriety with ChoicePoint. We are just a call away. Contact us directly 844.445.2563.
How to Verify Your Insurance?
To avail full benefits, you must verify your insurance at your selected rehab center first. Medicare provides coverage for drug and alcohol rehab, ensuring everyone has access to the necessary care.
Make the most of your time! The sooner you seek intervention, the more positive the outcome. Please take a moment to visit our website and verify your insurance now. Choose ChoicePoint as your dedicated partner in achieving long-term sobriety.
Medicare Inpatient Rehab Coverage- In A Nutshell
Imagine having a government health insurance plan that’s like a safety net for your health. Medicare has your back if you ever need to stay in inpatient rehab. With Medicare inpatient rehab coverage plans, patients feel no burden when paying for Addiction Treatment. But here’s the real game-changer: ChoicePoint is an Inpatient addiction rehab that accepts Medicare. Our DEA-certified doctors make your life so much easier. Call us now at 844.445.2563.
Medical Disclaimer:
ChoicePoint aims to improve the quality of life for people struggling with substance use disorder and mental health issues. Our team of licensed medical professionals research, edit and review the content before publishing. However, this information is not intended to be a substitute for professional medical advice, diagnosis, or treatment. For medical advice please consult your physicians or ChoicePoint's qualified staff.










Review Everything to Know About Medicare Inpatient Rehab Coverage.